There is no denying that mechanical and neurological pain has been one of the biggest burdens on productivity in the workplace and homestead. Surprisingly, pain effects more people than cancer, heart disease, and diabetes combined (1). 25.3 million American adults suffer from pain on a daily basis (20). 2/3 of office workers have experienced pain in the last 6 months and 1/4 of them believe it’s a normal part of the job (3). As a result, the pain is commonly untreated and the worker joins the other 100 million Americans suffering from chronic pain (3). The total costs attributable to low back pain alone in the United States were estimated at $100 billion in 2006, 2/3 of which were indirect costs of lost wages and productivity in the workplace (4).
Initially, as most patients with acute/subacute low back pain improve over time regardless of treatment, the American College of Physicians (ACP, 2017) recommends that clinicians and patients should select nonpharmacologic treatment with superficial heat, massage, acupuncture, or spinal manipulation. If pharmacologic treatment is desired, clinicians and patients should select nonsteroidal anti-inflammatory drugs or skeletal muscle relaxants (4).
Each of these suggested nonpharmacologic treatments in the acute/subacute phase can be implemented by an Osteopractic Physical Therapist. Moist hot packs are a standard in every Physical Therapy clinic. Massage can be performed in a variety of deep/soft tissue mobilization techniques such as Instrument-Assisted Soft Tissue Mobilization, body tempering, and static and dynamic cupping. Additionally, Osteopractors are certified in Functional Dry Needling/Electro Dry Needling, a scientific/western medicine version of acupuncture (5). Lastly, an Osteopractor is certified in Spinal Manipulation Therapy (5).
For patients with chronic low back pain, the ACP strongly recommends that clinicians and patients should initially select nonpharmacologic treatment with exercise, multidisciplinary rehabilitation, acupuncture, mindfulness-based stress reduction, tai chi, yoga, motor control exercise, progressive relaxation, electromyography biofeedback, low-level laser therapy, operant therapy, cognitive behavioral therapy, or spinal manipulation (4).
If the patient response to these interventions is insufficient, it would then be appropriate for clinicians and patients to consider pharmacologic treatment with nonsteroidal anti-inflammatory drugs, followed by tramadol or duloxetine (4). Clinicians should only consider opioids as an option for patients who have failed the aforementioned treatments and only if the potential benefits outweigh the risks for individual patients. Physicians are expected to have a discussion of the known risks and realistic benefits of opioids with their patients before prescribing them (4). Despite this recommendation, only 60.5% of patients nationally and 36.2% of patients in Massachusetts recall a discussion involving the risk of addiction with their physician (6).
Significant side effects in those taking opioids compared to placebo include constipation (16%), nausea (15%), dizziness/vertigo (8%), somnolence (9%), vomiting (5%), and pruritis (4%) (7). Other risks include dependence (3-26%),8 amnesia, insomnia, weight gain, sexual dysfunction, dry mouth, hyperhydrosis, urinary retention, cardiovascular issues, and death (9). Furthermore, concurrently taking an opioid with a benzodiazepine more than doubles a patient’s chance of hospital admission from an overdose (1.16% to 2.42%) (10). Despite the increased risk, 60% of patients who are taking opioids are also taking benzodiazepines or muscle relaxants (9). In addition, chronic use of opioids frequently results in decreased efficacy of the drug and opioid-induced hyperalgesia (9).
To better understand the shifting trends toward using opioids as a primary method for pain management, it is important to look at the statistical progression of this crisis and the methods taken to reverse the alarming direction of opioid negligence. In the 19th century, physician-scientists discovered that opiates such as morphine could reduce pain and chemist Felix Hoffmann developed aspirin from a substance in willow bark. However, it wasn’t until the past few decades that opioids became a mainstay for pain management (1).
In 1996 Purdue Pharm began marketing OxyContin extended-release (long-acting), a schedule 2 narcotic/opioid, to physicians and the media. Sales representatives claimed that the risk of addiction was less than 1% (12). However, based on a retroactive study of 1.25 million patients, the highest probabilities of continued opioid use at 1 (27.3%) and 3 years (20.5%) were seen among patients who received long-acting opioid treatment (13). Contrary to Purdue Harm’s claims, the prevalence of abuse ranking is as follows: OxyContin ≥ hydrocodone > other oxycodone > methadone > morphine > hydromorphone > fentanyl > buprenorphine (14).
Over the course of the first decade of the 21st century, prescription pain reliever sales and overdose death rates quadrupled (11). The admission rate for substance abuse treatment increased six-fold (11). Between 2002-2004, nearly 2/3 of heroin users reported non-medical use of opioids prior to initiation of heroin. That ratio increased to more than 4 of every 5 heroin users by 2008-2010 (15).
A 2007 meta-analysis on the efficacy of opioid use did not show a significant reduction in pain, compared to nonopiods or placebos (16). Despite the side effects and this lack of efficacy, an estimated 20% of patients presenting to physician offices with non-cancer pain symptoms or pain-related diagnoses (including acute and chronic pain) receive an opioid prescription (8).
In 2007, the ACP and American Pain Society (APS) released the first clinical guidelines for treatment of low back pain. It included patient education, self-symptom management, and encouraging the patient to remain active as the first line of options (17). If unsuccessful, they recommend acetaminophen or NSAIDs in conjunction with the aforementioned education (17). Emphasis is also placed on discussing the risks of addiction if prescribing opioids. Opioid analgesics or tramadol are only suggested if NSAIDs have failed or if the pain is debilitating (17). Next, a patient is instructed to undergo spinal manipulation, interdisciplinary rehab, exercise therapy, acupuncture, massage therapy, yoga, cognitive-behavioral therapy, or progressive relaxation (17).
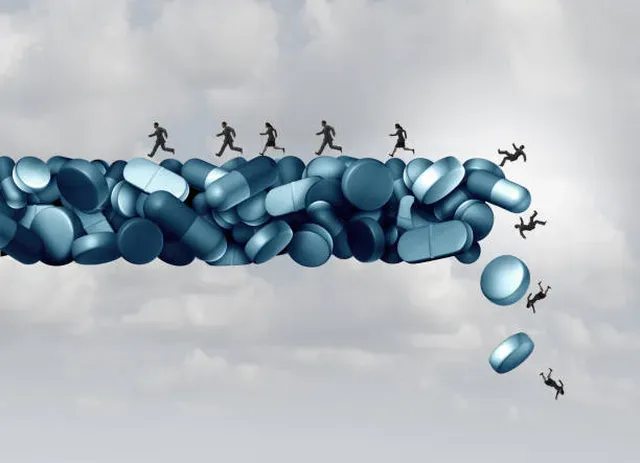
Despite these evidence-based guidelines, in 2012, 259 million prescriptions were written for opioids, which is more than enough to give every American adult their own bottle of pills (18). Even though Americans comprise under 5% of the world’s population, Americans consume 80% of the opioids prescribed worldwide (9). In 2013, the cost of medical care and substance abuse treatment for opioid addiction and overdose was an estimated $78.5 billion (19).
In 2014, 60.9% of drug overdose deaths in the US involved an opioid (28,647 deaths) (20). Between 2014-2015 alone, the age-adjusted opioid-involved death rate increased by 15.6%. (20). Drug overdoses are now the leading cause of death for those under 50 years of age in the US (9). More people are dying from drugs than HIV at the peak of its epidemic, auto accidents, and guns (9).
In 2015, more than 1/4 million children aged 12-17 were using non-medical opioids and nearly half of them were clinically addicted (8). From 2015 to 2016, opioid overdose deaths increased 27.7% (21). In 2016, The Centers for Disease Control and Prevention released a 50 page report outlining guidelines for prescribing opioids for chronic pain (22). In February 2018 Purdue Pharma announces it will cease marketing efforts to physicians after making $36 billion in sales (23).
Theoretically, opioids are prescribed to lower a patient’s pain and improve their functional ability. However, there was no significant difference in pain-related function compared to non-opioids over the course of 1 year (24). Furthermore, pain intensity was actually significantly less in the non-opioid group at 12 months (24). Even worse for opioids, the opioid group had twice the number of adverse side effects (1.8 vs. 0.9 symptoms) as the nonopioid group and was statistically significant (24).
Possible rationale for continued inflation of opioid prescriptions beyond best clinical judgement include initiation of pill mills where prescriptions are exchanged for cash, taking advantage of the addictive properties of opioids to ensure frequent return visits by patients, and naiveté of ACP or CDC guidelines (25). Further motivation to prescribe opioids are opioid company payments to physicians ($38,073,796 documented from August 2013-December 2015) (26). Other sources have noted pressure from hospital organizations on physicians to prescribe opioids in order to improve Hospital Consumer Assessment of Healthcare Providers and Systems scores, and thus increase hospital payments by the Centers for Medicare and Medicaid Services (9).
Prescribing physicians and pharmaceutical companies have been under scrutiny to implement changes and prevent drug-seeking behavior. Clinicians are on high alert to detect signs of abuse/misuse and to stay ahead of street-smart chemists who post on forums such as BlueLight.org. Abuse-deterrent opioids have sought to make modification of the drugs nearly impossible and avoid the sensation of euphoria or “the high.” Purdue’s version of the abuse-deterent OxyContin reduced addiction rates 27% among patients using OxyContin alone and 9% using OxyContin with other opioids (27). Additionally, pressure by Physicians for Responsible Opioid Prescribing seeks to have CMS remove pain-related questions from hospital ratings (9).
The DEA has taken swift action in the past several years shutting down pain clinics and charging healthcare professionals with fraud. In July 2017 alone, 412 individuals were charged or suspended for $1.3 billion in fraudulent opioid-related billing activities (28). Since a Florida legislative initiative that combined regulatory and criminal laws was put in place, there has been a significant decline in pill mills, opioid diversion, overdose deaths, and opioids. Criminal investigations as well as a prescription drug monitoring program has led to a heightened standard of care and restrictions for pain management clinics (29).
However, this leaves opioid-dependent patients without a segway to another clinician to manage their medications. This can lead to withdrawal, street-drug dependence, and even death (9). Abandoned patients must be strategically guided to medical professionals who will reduce the patient’s opioid dosage, address the psyche affiliated with the chronic pain, and transition the patient to a treatment of Suboxone or methadone, if necessary, as both have been shown to be effective (30,31). It is imperative that the psychology of a chronic pain patient be assessed and addressed. There has shown to be increased emotional distress, alteration in cognition, and reduced quality of life that much be understood from a biopsychosocial perspective (32).
Indicting physicians doesn’t seem to be an absolute solution, as the online pharmacy business is booming. 11,688 internet drug outlets are currently selling prescription medications to US patients (33). Of these, 11,142 (95.8%) were found to be operating out of compliance with state and federal laws (33). Many do not require a prescription, and about half are selling counterfeit painkillers and other fake medications. About 20 illegal online pharmacies are launched every day (33).
To further aid drug manufacturers/distributors with imposed regulatory obligations, the DEA added a new feature to its ARCOS Online Reporting System, a comprehensive drug reporting system that monitors the flow of controlled substances from their point of manufacture through commercial distribution channels to the point of sale at the dispensing/retail level (34).
The greatest focus should be on controlling the gate keeper in a multi-faceted approach. If patients are never exposed to an opioid in the first place, there will be less addiction, fewer opioids on the streets, and fewer people turning to heroin as a cheaper alternative. Because of the possibility of patients skewing their pain and functional outcome scores to demonstrate greater severity, it is also important to take into account other objective measures for pain and appropriateness for prescribing an opioid. One validated and reliable measure used to predict patient propriety for long-term opioid analgesic treatment for chronic noncancer pain is the DIRE (diagnosis, intractability, reliability with 4 parameters, and efficacy) scoring system (35,36). The benefit of the DIRE is that it also takes into account risk of opioid abuse/addiction by assessing variables of psychology, chemical health, and social support (35,36).
Additionally, Dr. Forest Tennant devised an evidence-based patient assessment to guide the prescribing of opioids (37). Tennant outlines signs of excess sympathetic discharge that are prevalent in uncontrolled pain as well as objective measures to determine uncontrolled pain and opioid overmedication, such as pulse rate, blood pressure, pupil diameter, and temperature of the extremities. Similar strategies are used in functional capacity evaluations to assess an individual’s ability to return to work (38).
Considering the accruing healthcare costs, number of deaths, and lack of proven functional efficacy of the opioid epidemic, it should be the ethical duty of prescribing physicians, insurance companies, government, and pharmaceutical companies to enforce such evaluation standards for prescribing opioids.
The greatest conundrum of all is that, despite all the advancements in medicine and knowledge of treatment methods for pain, opioids have even been an acceptable mainstay option. The leading cause of accidental deaths in the US are prescription drugs (39). Therefore, it is imperative that safer alternative options become blatantly apparent to those in pain and those who manage the pain of others.
Selective Adenylyl Cyclase Type 1 (AC1) inhibitors have been found in a natural product-like chemical database. They have been shown to reduce opioid dependence and inhibit allodynia (40). AC1 is is not required for acute pain responses and when AC1 is lacking, the behavioral response to inflammatory stimuli is practically eliminated (40). These are being researched as a potential alternative to opioids (40).
Cannabis can be an effective treatment for pain, greatly reduces the chance of dependence, and eliminates the risk of fatal overdose compared to opioid-based medications. In a study of nearly 2,800 patients, 97% were able to reduce their opioid intake and 81% found that cannabis alone was more effective in treating their pain than cannabis and opioids (39).
Dry Needling has been shown to be effective in low back pain (41), plantar heel pain (42), nonspecific neck pain (43), shoulder impingement (44), hip bursitis (equal to cortisone injection) (45), lumbar radiculopathy (46), bruxism/TMD pain (47), headaches (comparable to botox and lidocaine) (48), and fibromyalgia (pain, number of symptoms, general health, activity engagement, pressure pain threshold) (49) among others. Furthermore, in an independent case-series study of outpatient orthopedic patients with a variety of diagnoses, dry needling reduced pre to post treatment pain by nearly 4 points on the VAS.
Direct patient access compared with referred physical therapy is another solution to avoid early medication, unnecessary imaging, and pain that develops into a sub-acute to chronic issue (50). In a systematic review, significant results showed superior patient satisfaction, outcomes, along with a reduction in the number of physical therapy visits, imaging studies, medications prescribed, and additional medical visits from other disciplines (50).
There were also no additional harm or risk involved in the studies involving direct access (50).
Physical activity and exercise have proven to be an evidence-based alternative to reduce arthritic joint pain (51) neuropathic pain (52), risk of chronic back/neck/shoulder pain (53), headaches (54), and chronic low back pain (22).
High intensity laser therapy (HILT, 600-1,275nm, 1-75W) has shown effective with shoulder pain, chronic low back/neck pain (with exercise, lasting 3 months), acute neck pain (up to 22 weeks), cervical radiculopathy and spondylosis, myofascial pain syndrome of the trapezius, osteoarthritis, frozen shoulder, Bell’s palsy, shoulder impingement, lateral epicondylitis, carpal tunnel syndrome, and lumbar disc herniation (55). HILT is also an effective alternative to spinal surgery for chronic back pain in improving pain and function (55).
An additional safe alternative treatment approach, in spinal manipulation. Spinal manipulation has proven effective for low back pain (with exercise) in adolescents56 and non-specific low back pain in the adult population (57). Furthermore, treatment of neck pain with spinal manipulation was shown to be more effective than medication for 8, 12, 26, 26, and 52 weeks after intervention (58). Home exercises and advice are superior to medications at 26 weeks and not substantially different from spinal manipulation at all time points (58). Similarly, physical function improves in patients with lumbar spinal stenosis who received acupuncture but not in those receiving medication (59). This begs the question, why take the risk and medicate for mechanical pain at all?
In conclusion, there has been alarming rate of reactive opioid prescribing to combat pain with poor tracking and reduction of opioid intake. This has occurred despite the blatant risks, costs to the healthcare system, and proper education of patients. The alternative natural treatments and supporting research is well established as well as advocated by the same governing body of the individuals driving the opioid epidemic. Gate keepers must be held accountable, psychological and chemical treatment provided to those in chronic pain, and alternative natural methods must be made readily available to patients in pain so that the production and availability of opiates can be driven down. Lack of response to a single conservative treatment does not constitute failure as a multimodal approach tends to yield the best outcomes in numerous studies (4,17,22).
References
1. National Institutes of Health (NIH). (2010). NIH Fact Sheets – Pain Management. [online] Available at: https://report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=57 [Accessed 26 Mar. 2018].
2. National Institutes of Health (NIH). (2015). NIH analysis shows Americans are in pain. [online] Available at: https://www.nih.gov/news-events/news-releases/nih-analysis-shows-americans-are-pain [Accessed 26 Mar. 2018]
3. Productivity pains: New survey finds majority of american office workers experience physical pain at work. PR Newswire. Apr 10 2013. Available from: http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1324975600?accountid=15099.
4. Qaseem A, Wilt TJ, McLean RM, Forciea MA, . Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166:514–530. doi: 10.7326/M16-2367.
5. Spinal Manipulation Institute. (2018, January 17). Diploma in Osteopractic. Retrieved March 29, 2018, from https://spinalmanipulation.org/diploma-in-osteopractic/.
6. Hero, J. O., McMurtry, C., Benson, J., & Blendon, R. (2016). Discussing Opioid Risks With Patients to Reduce Misuse and Abuse: Evidence From 2 Surveys. Ann Fam Med, 14(6), 575-577.
7. Furlan, A. D., Sandoval, J. A., Mailis-Gagnon, A., & Tunks, E. (2006). Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ, 174(11), 1589-1594.
8. Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51). Retrieved from http://www.samhsa.gov/data/
9. Massion CT, M.D., Fugh-Berman A. Obfuscating opioid risks. The Women’s Health Activist. 2017;42(5):10-11. http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1943035093?accountid=15099
10. Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: Retrospective analysis. BMJ : British Medical Journal (Online). 2017;356. http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1877052093?accountid=15099. doi: http://dx.doi.org.libproxy.library.wmich.edu/10.1136/bmj.j760.
11. Paulozzi MD, Jones PharmD, Mack PhD, Rudd MSPH. Vital Signs: Overdoses of Prescription Opioid Pain Relievers – United State, 1999-2008. Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, Center for Disease Control and Prevention. 2011:60:5.
12. Van Zee, A. (2009). The promotion and marketing of oxycontin: commercial triumph, public health tragedy. Am J Public Health, 99(2), 221-227.
13. Shah, A., Hayes, C. J., & Martin, B. C. (2017). Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use – United States, 2006-2015. MMWR Morb Mortal Wkly Rep, 66(10), 265-269.
14. Cicero, Inciardi & Muñoz, 2005. Trends in Abuse of OxyContin® and Other Opioid Analgesics in the United States: 2002-2004. Journal of Pain, 6(10), pp.662–672.
15. Jones, C. M. (2013). Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers – United States, 2002-2004 and 2008-2010. Drug Alcohol Depend, 132(1-2), 95-100.
16. Martell, B. A., O’Connor, P. G., Kerns, R. D., Becker, W. C., Morales, K. H., Kosten, T. R. et al. (2007). Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med, 146(2), 116-127.
17. Chou, R., Qaseem, A., Snow, V., Casey, D., Cross, J. T., Shekelle, P. et al. (2007). Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med, 147(7), 478-491.
18. Centers for Disease Control and Prevention. (2014). Opioid Painkiller Prescribing, Where You Live Makes a Difference. Atlanta, GA: Centers for Disease Control and Prevention. Available at http://www.cdc.gov/vitalsigns/opioid-prescribing/
19. Florence, C. S., Zhou, C., Luo, F., & Xu, L. (2016). The Economic Burden of Prescription Opioid Overdose, Abuse, and Dependence in the United States, 2013. Med Care, 54(10), 901-906.
20. Rudd, R. A., Seth, P., David, F., & Scholl, L. (2016). Increases in Drug and Opioid-Involved Overdose Deaths – United States, 2010-2015. MMWR Morb Mortal Wkly Rep, 65(5051), 1445-1452.
21. Vivolo-Kantor, A. M., Seth, P., Gladden, R. M., Mattson, C. L., Baldwin, G. T., Kite-Powell, A. et al. (2018). Vital Signs: Trends in Emergency Department Visits for Suspected Opioid Overdoses – United States, July 2016-September 2017. MMWR Morb Mortal Wkly Rep, 67(9), 279-285.
22. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1–49. DOI: http://dx.doi.org/10.15585/mmwr.rr6501e1.
23. Marketplace staff and associated press. Ocycontin maker Purdue Pharma to stop marketing opioids to doctors. February 10, 2018. https://www.marketplace.org/2018/02/10/health-care/uncertain-hour/oxycontin-maker-purdue-pharma-stop-marketing-opioids-doctors
24. Krebs, E. E., Gravely, A., Nugent, S., Jensen, A. C., DeRonne, B., Goldsmith, E. S. et al. (2018). Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA, 319(9), 872-882.
25. Dineen KK, DuBois JM. Between a Rock and a Hard Place: Can Physicians Prescribe Opioids to Treat Pain Adequately While Avoiding Legal Sanction? American journal of law & medicine. 2016;42(1):7-52.
26. Hadland, Scott E, MD,M.P.H., M.S., Krieger MS, B.S., Marshall BDL, PhD. Industry payments to physicians for opioid products, 2013–2015. Am J Public Health. 2017;107(9):1493-1495. http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1938529470?accountid=15099. doi: http://dx.doi.org.libproxy.library.wmich.edu/10.2105/AJPH.2017.303982.
27. Coplan & Kadakia, 2015. Changes in diagnosed addiction rates in patients prescribed opioids after introduction of OxyContin with abuse-deterrent properties. Drug and Alcohol Dependence, 156, p.e48.
28. DEA Public Affairs. “National Health Care Fraud Takedown: Charges Against Over 412 Individuals Responsible for $1.3 Billion in Fraud.” DEA.gov / Headquarters News Releases, 07/13/17, 13 July 2017, www.dea.gov/divisions/hq/2017/hq071317.shtml
29. Gau JM, Brooke EJ. An assessment of the impact of a multipronged approach to reducing problematic pain clinics in florida. J Drug Iss. 2017;47(2):185-204. http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1875399257?accountid=15099. doi: http://dx.doi.org.libproxy.library.wmich.edu/10.1177/0022042616681273.
30. McKeganey, N., Russell, C., & Cockayne, L. (2013). Medically assisted recovery from opiate dependence within the context of the UK drug strategy: methadone and Suboxone (buprenorphine-naloxone) patients compared. J Subst Abuse Treat, 44(1), 97-102.
31. Suboxone versus Methadone for the Treatment of Opioid Dependence: A Review of the Clinical and Cost-effectiveness [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2013 Nov 14. APPENDIX 4, Main Study Findings and Authors’ Conclusions. Available from: https://www.ncbi.nlm.nih.gov/books/NBK195150/
32. Roditi, D., & Robinson, M. E. (2011). The role of psychological interventions in the management of patients with chronic pain. Psychol Res Behav Manag, 4, 41-49.
33. The National Association of Boards of Pharmacy. Internet Drug Outlet Identification Program Progress Report for State and Federal Regulators. August 2017. 1-14.
34. DEA Public Affairs. “DEA creates new resource to help distributors avoid oversupplying opioids.” DEA.gov / Headquarters News Releases, 02/14/18, Accessed 28 March 2018. https://www.dea.gov/divisions/hq/2018/hq021418.shtml.
35. Belgrade, M. J., Schamber, C. D., & Lindgren, B. R. (2006). The DIRE score: predicting outcomes of opioid prescribing for chronic pain. J Pain, 7(9), 671-681.
36. Zweifler, J. A. (2012). Objective evidence of severe disease: opioid use in chronic pain. Ann Fam Med, 10(4), 366-368.
37. Tennant, F. (june 2008). Using Objective Signs of Severe Pain to Guide Opioid Prescribing. Pain Treatment Topics, 1-6. Retrieved March 27, 2018, from Pain-Topics.org. 38. Chen JJ. Functional capacity evaluation & disability. Iowa Orthop J (2007) 27:121–7. Reiman A, Welty M, Solomon P.
39. Cannabis as a Substitute for Opioid-Based Pain Medication: Patient Self-Report. Cannabis and Cannabinoid Research. 2017;2(1):160-166. doi:10.1089/can.2017.0012.
40. Watts VJ. (2018) Selective Adenylyl Cyclase Type 1 Inhibitors as Potential Opioid Alternatives For Chronic Pain. Neuropsychopharmacology 43:215-216.
41. Liu L, Huang QM2 Liu QG, Thitham N, Li LH, Ma YT, Zhao JM. Evidence for Dry Needling in the Management of Myofascial Trigger Points Associated With Low Back Pain: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil. 2018 Jan;99(1):144-152.e2. doi: 10.1016/j.apmr.2017.06.008. Epub 2017 Jul 8.
42. Cotchett MP, Munteanu SE, Landorf KB. Effectiveness of trigger point dry needling for plantar heel pain: A randomized controlled trial. Phys Ther. 2014;94(8):1083-94. http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1550961578?accountid=15099
43. Cerezo-Tellez E et al. (2016) Effectiveness of dry needling for chronic nonspecific neck pain: a randomized, single-blinded, clinical trial. Pain 157:1905-17
44. Kamali, F., Sinaei, E., & Morovati, M. (2018). Comparison of Upper Trapezius and Infraspinatus Myofascial Trigger Point Therapy by Dry Needling in Overhead Athletes With Unilateral Shoulder Impingement Syndrome. J Sport Rehabil, 1-24.
45. Brennan KL et al. (2017) Dry Needling Versus Cortisone Injection in the Treatment of Greater Trochanteric Pain Syndrome: A Noninferiority Randomized Clinical Trial. J Orthop Sports Phys Ther 47:232-239.
46. Mahmoudzadeh A et al. (2016) The effect of dry needling on the radiating pain in subjects with discogenic low-back pain: A randomized control trial. J Res Med Sci 21:86.
47. Blasco-Bonora PM and Martin-Pintado-Zugasti A. (2017) Effects of myofascial trigger point dry needling in patients with sleep bruxism and temporomandibular disorders: a prospective case series. Acupunct Med 35:69-74.
48. Kietrys, D.M., Palombaro, K.M. & Mannheimer, J.S. Curr Pain Headache Rep (2014) 18: 437. https://doi-org.libproxy.library.wmich.edu/10.1007/s11916-014-0437-0.
49. Casanueva B, Rivas P, Rodero B, Quintial C, Llorca J, González-gay M,A. Short-term improvement following dry needle stimulation of tender points in fibromyalgia. Rheumatol Int. 2014;34(6):861-6. http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1526108297?accountid=15099. doi: http://dx.doi.org.libproxy.library.wmich.edu/10.1007/s00296-013-2759-3.
50. Ojha HA, Snyder RS, Davenport TE. Direct access compared with referred physical therapy episodes of care: A systematic review. Phys Ther. 2014;94(1):14-30. http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/1494384704?accountid=15099.
51. Fewer Opioids, More Exercise for Severe Joint Pain From Arthritis . JAMA. 2016;316(20):2079. doi:10.1001/jama.2016.16667.
52. Opioids; new findings from kagoshima university in the area of opioids reported (the effect of exercise frequency on neuropathic pain and pain-related cellular reactions in the spinal cord and midbrain in a rat sciatic nerve injury model). Obesity, Fitness & Wellness Week. Mar 03 2018:3915. Available from: http://libproxy.library.wmich.edu/login?url=https://search-proquest-com.libproxy.library.wmich.edu/docview/2007541012?accountid=15099.
53. Nilsen TI et al. (2011) Physical exercise, body mass index, and risk of chronic pain in the low back and neck/shoulders: longitudinal data from the Nord-Trondelag Health Study. Am J Epidemiol 174:267-73.
54. Baillie, L.E., Gabriele, J.M. & Penzien, D.B., 2014. A Systematic Review of Behavioral Headache Interventions With an Aerobic Exercise Component. Headache: The Journal of Head and Face Pain, 54(1), pp.40–53.
55. White PF et al. (2017) Use of electroanalgesia and laser therapies as alternatives to opioids for acute and chronic pain management. F1000Res 6:2161
56. Evans R et al. (2018) Spinal Manipulation and Exercise for Low Back Pain in Adolescents: A Randomized Trial. Pain.
57. Ruddock JK, Sallis H, Ness A, Perry RE. Spinal Manipulation Vs Sham Manipulation for Nonspecific Low Back Pain: A Systematic Review and Meta-analysis. Journal of Chiropractic Medicine. 2016;15(3):165-183. doi:10.1016/j.jcm.2016.04.014.
58. Bronfort G et al. (2012) Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Ann Intern Med 156:1-10.
59. Oka H et al. (2018) A comparative study of three conservative treatments in patients with lumbar spinal stenosis: lumbar spinal stenosis with acupuncture and physical therapy study (LAP study). BMC Complement Altern Med 18:19.