What is lymphedema?
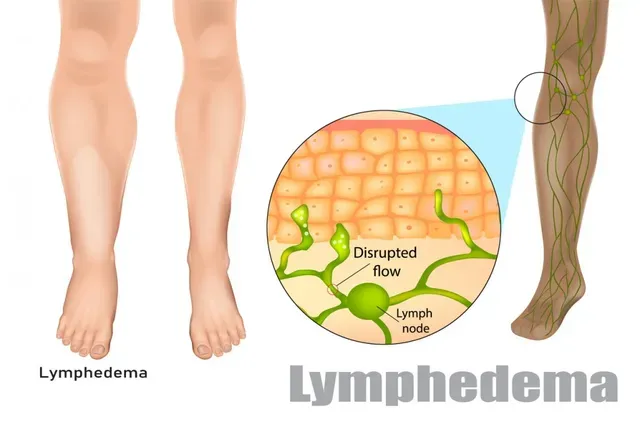
If you have been through cancer treatment, especially breast cancer treatments, you may heard the term lymphedema. When large numbers of lymph nodes are removed the risk for lymphedema increases. For those unfamiliar with the term, lymphedema is a chronic disease where the extracellular fluid is retained and is protein-rich, creating a high risk of skin complications. It causes chronic inflammation, an increase in fat tissue and superficial skin changes (like hardening) and if not taken care of increases the risk of skin infections like cellulitis. Swelling does not reduce with elevation and there is usually a feeling of heaviness to the body part. Lymphedema can occur in one or multiple areas of the body and comes on gradually (1, 2).
How can physical therapy help me?
Therapists can be trained in what is known as Complete Decongestive Therapy(CDT). This is made up of 4 parts: Manual Lymph Drainage-type of “massage”, compression wrapping, low impact exercise, and self care.
- Manual Lymph Drainage(MLD) is a massage technique that increases the lymphatic flow in the proper directions to decrease the size of the body part being decongested.
- Compression wrapping with specific short stretch bandages or utilization of compression garments further aids in maintaining the decrease in size, and aids in continual lymph decongestion thru the pressure gradient on the skin.
- The low impact exercise following the MLD and compression further aids the movement of lymph.
- The type of exercise is low impact, repetitive, rhythmic and non-resistive (no weights) emphasizing the full range of motion.
- The final piece of the CDT puzzle is self-care, specifically education special skin care needs.
How do I know if I have edema(swelling) or lymphedema?
A trained therapist will know how to test for the difference. Edema is a symptom where fluid accumulates in extracellular space and after successful treatment there is complete resolution. Lymphedema is a chronic disease. However, even with post-surgical or post injury edema, a therapist trained in MLD can still help. The techniques of CDT work exceptionally well with post-surgical or post-injury edemas!
A Note to those fighting Breast Cancer:
You are those highest at risk for developing lymphedema because of the location of the cancer and cancer treatment areas that are so close to large pockets of lymph nodes in the body(armpit region) (3,4).
Physical Therapy can offer 3 Phases of treatment:
Phase 1: Pre-Treatment Diagnosis: Seeing a Certified Lymphedema Therapist (CLT) prior to surgery is EXTREMELY helpful to take initial baseline measurements of the upper extremities and provide education to catch any changes early to avoid body part enlargement. Unfortunately, this service is not covered by insurance yet, however many offices do offer this as a complimentary service.
Phase 2: Pre-Radiation or Pre-Chemotherapy Phase: If a patient has difficulty positioning arm for radiation, we can mobilize scar tissue and increase the range of motion to allow the radiation position to be obtained. (We generally do not do treatments DURING radiation, the skin needs to be fully healed, appx. 6-8weeks, to begin Phase 3)
Phase 3: Post Radiation Phase: breast cancer patients- your shoulders will get tight from radiation fibrosis, scar tissue adhesions. Physical therapy can help to increase your shoulder function and decrease the pain of the shoulder and breast tissue as we work on the fibrotic and scar tissue. We will continually take girth/volume measurements to monitor for lymphedema/edema, aid in compression garment fitting/compression pumps if needed and continue education on lymphedema and special skin care. Breast cancer survivors who have received chemotherapy are 5 times more likely to experience a fracture due to risk of treatment induced osteoporosis. Physical therapy can provide guided weight bearing exercises can slow down the bone loss (5,6).
Other diagnoses that can benefit from CDT and/or MLD:
- Chronic Venous Insufficiency
- Post-Surgical Swelling from Joint Surgeries
- Lipedema
- And others…Contact your preferred Physical Therapist Office to see if they can help!
REFERENCES:
1. Klose, Gunter. 2021. Klose Training Lymphedema Certification Manual.
2. Foeldi M, et al. 2003. (First American Edition). Textbook of Lymphology. Munich, Germany: Urban & Fischer.
3. American Cancer Society (ACS). Cancer.org. Assessed in 2013.
4. Williams AF, Franks PJ, Moffatt CJ. Lymphoedema: Estimating the size of the problem. Palliat Med. 2005;19(4): 300-313.
5. Schmitz, K. 2011. “Physical Activity and Breast Cancer Survivorship.” In Physical Activity and Cancer: Recent Results in Cancer Research. Courneya, KS, Freidenreich CM, eds., Chapter 8. Springer-Verlag Berlin Heidelberg.
6. Ewertz M, Jensen AB. 2011. Late Effects of Breast Cancer Treatment and Potentials for Rehabilitation. Acta Oncologica 50:187-193.